SLIPKNOT TOUR DATES IN 2015
SLIPKNOT TOUR DATES 2015
25-Apr Fort Rock Festival
Fort Myers, FL
26-Apr Welcome to Rockville Festival
Jacksonville, FL
29-Apr Pensacola Civic Center
Pensacola, FL
w/ Hatebreed
30-Apr Champions Square - Superdome
New Orleans, LA
w/ Hatebreed
2-May Oak Mountain Amphitheatre
Pelham, AL
w/ Hatebreed
3-May Carolina Rebellion Concord, NC
5-May Knoxville Coliseum
Knoxville, TN
w/ Hatebreed
8-May U.S. Cellular Coliseum
Bloomington, IL
w/ Hatebreed
9-May Northern Invasion Somerset, WI
10-May U.S. Cellular Center
Cedar Rapids, IA
w/ Hatebreed
12-May Erie Insurance Arena
Erie, PA
w/ Hatebreed
13-May The Pavilion at Montage Mountain
Scranton, PA
w/ Hatebreed
15-May Rock On The Range
Columbus, OH
16-May Van Andel Arena
Grand Rapids, MI
w/ Hatebreed
5-Jun Rock Im Park
Nuremberg, Germany
5-Jun Rock Am Ring 2015
Mendig, Germany
6-Jun FortaRock Festival
Nymegen, Netherlands
7-Jun Rock Am Ring 2015
Mendig, Germany
7-Jun Rock Im Park
Nuremberg, Germany
9-Jun Impact Festival
Łódź, Poland
12-Jun Download Festival
Derby, United Kingdom
14-Jun Novarock
Nickelsdorf, Austria
16-Jun Rock in Roma
Rome, Italy
19-Jun Hellfest Clisson, France
20-Jun Graspop Metal Meeting
Dessel, Belgium
24-Jul Cruzan Amphitheatre
West Palm Beach, FL
w/ Lamb of God, Bullet...
25-Jul MIDFLORIDA Credit Union Amphitheatre
Tampa, FL
w/ Lamb of God, Bullet...
26-Jul Aaron's Amphitheatre
Atlanta, GA
w/ Lamb of God, Bullet...
28-Jul DTE Energy Music Theatre
Detroit, MI
w/ Lamb of God, Bullet...
29-Jul Darien Lake PAC
Darien Center, NY
w/ Lamb of God, Bullet...
31-Jul Spac
Saratoga Springs, NY
w/ Lamb of God, Bullet...
1-Aug Nikon at Jones Beach
Wantagh, NY
w/ Lamb of God, Bullet...
2-Aug Xfinity Theatre
Hartford, CT
w/ Lamb of God, Bullet...
4-Aug Xfinity Center
Winthrop, MA
w/ Lamb of God, Bullet...
5-Aug PNC Bank Arts Center
Holmdel, NJ
w/ Lamb of God, Bullet...
6-Aug First Niagara Pavilion
Pittsburgh, PA
w/ Lamb of God, Bullet...
8-Aug Molson Canadian Amphitheatre
Toronto, Canada
w/ Lamb of God, Bullet...
11-Aug Jiffy Lube Live
Washington, DC
w/ Lamb of God, Bullet...
12-Aug Farm Bureau Live
Virginia Beach, VA
w/ Lamb of God, Bullet...
14-Aug Klipsch Music Center
Indianapolis, IN
w/ Lamb of God, Bullet...
15-Aug First Midwest Bank Amp
Chicago, IL
w/ Lamb of God, Bullet...
16-Aug Hollywood Casino Amphitheatre
Saint Louis, MO
w/ Lamb of God, Bullet...
19-Aug Red Rocks Amphitheatre
Denver, CO
w/ Lamb of God, Bullet...
21-Aug USANA Amphitheatre
Salt Lake City, UT
w/ Lamb of God, Bullet...
24-Aug Rogers Arena
Vancouver, Canada
w/ Lamb of God, Bullet...
26-Aug Concord Pavilion
Concord, CA
w/ Lamb of God, Bullet...
28-Aug MGM Resort Festival Lot
Las Vegas, NV
w/ Lamb of God, Bullet...
29-Aug Ak-Chin Pavilion
Phoenix, AZ
w/ Lamb of God, Bullet...
30-Aug Isleta Amphitheater
Albuquerque, NM
w/ Lamb of God, Bullet...
2-Sep Austin360 Amphitheater
Austin, TX
w/ Lamb of God, Bullet...
4-Sep Cynthia Woods Mitchell Pavilion
Houston, TX
w/ Lamb of God, Bullet...
5-Sep Gexa Energy Pavilion
Dallas, TX
w/ Lamb of God, Bullet...
25-Sep Rock in Rio Rio De Janeiro, Brazil
Linkin Park have released video of the moment frontman Chester Bennington broke his ankle.
Latest episode of LPTV features moment frontman broke ankle playing basketball
Linkin Park have released video of the moment frontman Chester Bennington broke his ankle.
The band were forced to call off a run of shows in January after the incident, which took place while he and colleagues were playing basketball.
The clip, part of the latest episode of LPTV, shows Bennington on the ground, writing in pain. He explains: “I landed on the bottle. I was in full lay-up, I landed on the water bottle and my ankle turned.”
He’s treated by a first aider then taken away in a wheelchair with his leg strapped up.Bandmates later reported he was making a fast recovery.
Meanwhile, the vocalist has spoken of his delight that he can tour with Stone Temple Pilots without adding his own name to the title.
He replaced Scott Weiland in 2013, but legal issues apparently forced them to be billed as Stone Temple Pilots With Chester Bennington.
Now he tells AltWire: “It’ll be fun to go out as just Stone Temple Pilots. It really bothered me to see ‘Stone Temple Pilots With Chester Bennington.’ I’m glad that’s over.”
They’re currently working on a full album to follow their High Rise EP.
One Man Found a Mysterious Box in a Dumpster – What Was in it Was Absolutely Baffling
http://howtoexitthematrix.com/2015/03/17/one-man-found-a-mysterious-box-in-a-dumpster-what-was-in-it-was-absolutely-baffling/

































One Man Found a Mysterious Box in a Dumpster – What Was in it Was Absolutely Baffling
THE BOX WAS HANDMADE FROM WOOD, FIT WITH HINGES, A HANDLE AND A PAIR OF LOCKS.

FROM WHAT WAS WRITTEN HERE, IT APPEARS THAT THE AUTHOR HAD AN EXPERIENCE THAT WAS DEFINITELY NOT FROM HERE.

A HAND-DRAWN TABLE OF THE ELEMENTS.

THIS PATENT IS NOT FILED WITH THE UNITED STATES PATENT OFFICE – BUT THE DRAWINGS ARE REMARKABLY DETAILED. BUT THIS IS NOT THE WEIRDEST PART…

THIS DRAWING WAS DATED 1939 – WHY WOULD SOMEONE DISCARD THIS?

ODDLY, THIS MAP SHOWS AIR TRAVEL ROUTES.

A LOT OF THE MAPS ARE HAND-DRAWN WITH A “CENTER” NOTED ON IT.

THE MAPS REPRESENT AERIAL PATTERNS AND/OR ROUTES OF SOME TYPE.

THERE WERE QUITE A FEW OF THE MAPS

AND THE MYSTERY CONTINUES…

A NOTE PERHAPS FROM THE PREVIOUS OWNER

ANOTHER MAP WITH A “CENTER” ON IT

A PIECE OF THE PAST – A NOTE FROM A VERY OLD VETERANS AFFAIRS OFFICE

THE ARTIST DEPICTS AN EVENT FROM TAMPA, FL IN 1977. HE NOTES THE EVENT TO BE EXTRATERRESTRIAL IN NATURE

ODD TO SEE EXTRATERRESTRIAL UFO ON THE SAME PAGE WITH ANGELIC-LOOKING CREATURES

DRAWING OF AN ENTITY

A SLIGHT SUMMARY OF THE EVENTS

GEOMETRIC SHAPES THAT ARE RELATED

ANOTHER DRAWING OF ONE OF THE ENTITIES – LOOKS STRANGELY LIKE SOMETHING OUT OF THE BIBLICAL BOOK OF EZEKIEL

AN ADDITIONAL SKETCH OF THE SAME BEING

BEINGS FROM THE SIDE VIEW

THE ARTIST WAS FIXATED ON THESE CREATURES FOR SOME TIME

WAS THIS A DREAM OR DID THIS REALLY HAPPEN?

ONE MIGHT SAY THIS LOOKS LIKE WHEELS WITHIN WHEELS, WINGS FULL OF EYES AND CREATURES WITH 4 HEADS (MAN, OX, EAGLE AND LION) FROM THE BOOK OF EZEKIEL

THE DRAWINGS SEEM TO MIX BIBLICAL AND EXTRATERRESTRIAL VISIONS

A CLOSE-UP OF THE CORNER

THE DETAILS OF THIS DRAWING INCLUDE SOME OF THE PATENT DRAWINGS SEEN EARLIER

A DIFFERENT VIEW OF ONE OF THE PATENT DRAWINGS

IT APPEARS THAT THESE NEW TRAIN WHEELS MIGHT HAVE COME FROM THE TRAIN HE DREW EARLIER

WHAT ARE YOUR THOUGHTS?


Whatever your conclusion – someone who was working too hard, a drug-induced vision, or a true extra-terrestrial experience…it sure is a puzzle. Unfortunately, we cannot ask the artist and know for sure. All we know is that this person experienced something very odd. Perhaps he knows something that we don’t.
Physician’s Organization in Canada Releases Guidelines for Prescribing Medical Cannabis for Pain

 Arielle GerardDecember 31, 2014
Arielle GerardDecember 31, 2014Prescribing Patients Medical Cannabis for Pain
conditions recommended for use circumstances under which medical cannabis should not be recommended circumstances under which caution should be taken when recommending medical cannabis use dosing
Guidelines For Canadian Physicians
The guidelines are as follows, taken verbatim from the guidelines set forth in the study:
Smoked cannabis might be indicated for patients with severe neuropathic pain conditions who have not responded to adequate trials of pharmaceutical cannabinoids and standard analgesics (level II evidence).
Smoked cannabis is contraindicated in patients who are 25 years of age or younger (level II evidence); who have a current, past, or strong family history of psychosis (level II evidence); who have a current or past cannabis use disorder (level III evidence); who have a current substance use disorder (level III evidence); who have cardiovascular or respiratory disease (level III evidence); or who are pregnant or planning to become pregnant (level II evidence).
It should be used with caution in patients who smoke tobacco (level II evidence), who are at increased risk of cardiovascular disease (level III evidence), who have anxiety or mood disorders (level II evidence), or who are taking higher doses of opioids or benzodiazepines (level III evidence).
Cannabis users should be advised not to drive for at least 3 to 4 hours after smoking, for at least 6 hours after oral ingestion, and for at least 8 hours if they experience a subjective “high” (level II evidence).
The maximum recommended dose is 1 inhalation 4 times per day (approximately 400 mg per day) of dried cannabis containing 9% delta-9-tetrahydrocannabinol (level III evidence).
Physicians should avoid referring patients to “cannabinoid” clinics (level III evidence).
Evaluation/Explanation of Guidelines
Generally, the regulations seem reasonable considering that the recommendations are specifically for patients with chronic non-cancer pain who are smoking their medical cannabis.
Adolescent Use
It is currently unclear whether or not cannabis use, when started in adolescence, leads to impairment in brain development. While some studies have found a link between early cannabis use and morphological brain changes, others which are more carefully controlled have found no link.
Due to the fact that cannabis use may interrupt normal brain development, children and adolescents should avoid use of cannabis unless it is deemed by a physician, in rare cases, that the potential benefits of use outweigh the risks.
History of Psychosis and Anxiety/Mood Disorders
While a link between cannabis use and certain mental health disorders has been noted, a cause-effect relationship has never been assessed. In other words, there is no definitive evidence that cannabis use actually causes mental health disorders, and the link is potentially due to the fact that those predisposed to certain mental health disorders may choose to self-medicate with cannabis.
Psychosis
Due to its classification as a hallucinogen, cannabis use may exacerbate certain mental health disorders, such as psychosis. Additionally, during intoxication with use of cannabis strains with higher levels of delta-9-tetrahydrocannabinol (THC), users (especially those who are inexperienced) may experience paranoia and emotional discomfort. Therefore, avoiding use in those with a past or family history of psychosis is recommended.
Anxiety and Mood Disorders
Many patients find that cannabis helps to relieve their anxiety. Regarding mood disorders, a recent study found that those with baseline major depressive disorder were more likely to begin cannabis use, but that cannabis use was not linked to an increased likelihood of having major depressive disorder. Additionally and interestingly, while “weekly to almost daily” cannabis use was associated with an increased likelihood of having baseline borderline personality disorder, daily use was not; there was also no link found between baseline borderline personality disorder and an increased likelihood to begin using cannabis. However, for those with mood and anxiety disorders, caution should be taken in using medical cannabis, for similar reasons as those noted at the beginning of this section.
Lung/Heart/Vascular Problems
Cannabis use may result in heart and vascular (i.e. blood vessel) problems in some patients (e.g. low blood pressure which can be harmful in certain diseases/disorders, potential increased risk of heart attack). While there is some evidence that cannabis use increases the risk ofstroke, other evidence has suggested a decreased risk of stroke with a history of past cannabis use. Due to the fact that the impact of cannabis use on heart/vascular problems is not fully understood, use should be avoided by individuals with these health issues.
Additionally, smoking cannabis can irritate the airways and lungs. While a recent Harvard study found that low to moderate frequency of cannabis use does not result in decreased lung function in the general population, for those (1) with health issues related to the lung or (2) who also smoke tobacco (which is highly damaging to the lungs and strongly linked to the development of cancer of various organs), smoked cannabis should be avoided. Vaporization and ingestion methods are an alternative form of cannabis administration that will help to prevent additional lung damage.
Substance Abuse Disorders
Cannabis use should be avoided for patients with past cannabis or other substance abuse disorders in most cases, due to the potential for continuing or reestablishing dependence issues.
Pregnancy
Although use of cannabis itself during pregnancy is not definitively linked to future health issues in those exposed in the womb, it has been linked to inattention, impulsivity, and hyperactivity. However, in one 1991 study of Jamaican mothers who had used cannabis during pregnancy, no differences between children exposed to cannabis in the womb vs. children unexposed to cannabis in the womb were found by age 5 (except at day 30 post-birth, when infants who had been exposed to cannabis in the womb actually had better scores on a neonatal behavioral assessment scale). While (1) the majority of studies on how cannabis use during pregnancy impacts the fetus/child have focused on heavy rather than moderate use and (2) the link between behavioral/cognitive issues in children who were exposed to cannabis in the womb may be an issue of general parental behavior/responsibility rather than cannabis use itself, cannabis use during pregnancy still carries the risk of harm. Use of cannabis while pregnant may lead to bone formation abnormalities and stunted height of the fetus, and potentially cognitive and behavioral deficits, and smoked cannabis still contains cancer-causing/destructive compound. Therefore, cannabis use should be avoided during pregnancy to avoid any potential developmental, behavioral, and cognitive dysfunction that may result from cannabis use.
Driving
Cannabis use may cause slowed complex reaction times and a skewing of perception of time and space. Therefore, driving while under the influence of cannabis should be avoided. However, the implications of driving under the influence of cannabis is more nuanced than the issue of those driving under the influence of alcohol, partially because medical cannabis users still need to function in their daily lives.
While cannabis use has been shown to increase lateral (side-to-side) motion within a lane, it has not been shown to impair handling, maneuvering, or turning. Some studies of drivers who have smoked cannabis alone (i.e. no additional alcohol impairment) have shown that they are no more likely than drivers who are sober to be involved in a fatal car accident, and a federal report released in February 2015 found no link between testing positive for THC (which can occur during intoxication, but also days after intoxication) and an increased risk of car crashes. This is partially due to the fact that people who have consumed cannabis tend to drive slower, leave more space between their car and the car in front of them, and are less likely to pass other cars. Alcohol has the opposite effect, and is known to greatly increase the chance of fatal accidents. Additionally, intoxicated drivers under the influence of cannabis tend to be more aware of their impairment than intoxicated drivers under the influence of alcohol, and some cannabis users who have often practiced driving under the influence show no changes in their driving behavior under the influence, as compared to driving behavior while sober. Driving under the influence of low doses (e.g. 0-4 inhalations/day of cannabis with <9% THC–often all that is needed for medical use [e.g. pain relief]) is more similar to driving under the influence of Benadryl (which should also be avoided), rather than alcohol.
However, cannabis with higher concentrations of THC or multiple inhalations may lead to more significant impairment. Due to (1) slowed reaction times, (2) skewing of time/space perception, and (3) increased lateral lane motion under cannabis intoxication, and (4) the inability for medical users to objectively assess whether or not they are experienced drivers under the influence of cannabis, those using cannabis should not drive while experiencing intoxication (i.e. psychoactive effects) and should follow the recommendations outlined in these guidelines.
Note: Driving under the influence of both alcohol and cannabis use simultaneously is more dangerous than driving under the influence of either alone, and should always be avoided.
Conclusion
Overall, the guidelines provided by the College of Family Physicians of Canada are well-informed, evidence-based, reasonable, and progressive. While some may find that the guidelines attempt to put too many limitations on medicinal cannabis use, safety considerations, appropriately, seem to be at the forefront of their creation. Potential improvements to the guidelines could include (1) recommendations for diseases/symptoms, other than neuropathic pain, that may be benefited by medical cannabis use, and (2) discussion of additional methods of delivery, including vaporization and ingestion, which would be useful for all practitioners, but especially for those who are uncomfortable recommending their patients smoke.
The introduction of reasonable guidelines surrounding medical cannabis use by established physician’s organizations, in Canada and worldwide, will likely help to decrease the stigma associated with/increase knowledge about medical cannabis use, especially for older and more conservative patients and physicians, thereby increasing access to this relatively safe treatment option for those in need.
READ MORE OF THE ARTICLE HERE http://www.medicaljane.com/2014/12/31/physicians-organization-in-canada-releases-guidelines-for-prescribing-medical-cannabis-for-pain/
Cannabis-Based Medicines As Potential Treatments For Traumatic Brain Injuries

 Arielle Gerard October 18, 2014
Arielle Gerard October 18, 2014THC Helps Prevent Death From Traumatic Brain Injury
In a recent study titled “Effect of Marijuana Use on Outcomes in Traumatic Brain Injury” and published in The American Surgeon, researchers found that patients who had detectable levels of THC in their bodies were less likely than those who did not to die as a result of traumatic brain injury (TBI). The retrospective study examined the data of 446 cases of traumatic brain injuries over a three year period, involving patients who had been treated at Harbor-UCLA Medical Center in Torrance, CA.
Overall, 18.4% of patients traumatic brain injury in the sample had toxicology reports positive for the presence of THC, and the death rate for all cases examined was 9.9%. After adjusting for differences that may confound results (such as age, gender, and classification of injury), the death rate for TBI patients with THC-negative toxicology reports (i.e. without detectable levels of THC in their body) was 11.5%, but for traumatic brain injury patients with THC-positive reports was only 2.4%. Therefore, the survival of THC-positive TBI patients was approximately 80 times more than the survival of THC-negative TBI patients.

Interpretation Of The Study’s Results
The fact that this was a retrospective analysis, as opposed to a double-blind, placebo-controlled, randomized trial, limits the ability to determine a cause-effect relationship from the study (i.e. it cannot be determined from this study alone that THC is the direct cause of the decreased rate of death from TBI). Additionally, the frequency of cannabis use of the THC-positive patients and the method of delivery used by the traumatic brain injury patients (e.g. smoking, vaporizing, ingesting) was unknown.
“…therefore, the survival of THC-positive TBI patients was approximately 80 times more than the survival of THC-negative TBI patients.”
According to a Reuters article on the study, “One concern with the study, according to [Dr. David] Plurad (one of the study’s authors), is that the test for THC could not distinguish between occasional and regular users. A person could test positive after having used marijuana days or even weeks before.” This is largely due to the fact that THC is fat-soluble, and can therefore accumulate in your fat cells instead of being immediately excreted by the body, like water-soluble compounds.
Plurad also states that while similar studies conducted in the past found that alcohol was protective from TBI death, the presence/absence of THC in these studies was not controlled for. Therefore, the potential exists (“potential” being the key word) that the patients who had detectable levels of alcohol in their body in these studies also had THC in their system, which is what actually led to the neuroprotective results. Because of this, the validity of these past studies’ results may be limited. Additionally, the researchers in the currently reviewed study also examined the effect of alcohol on traumatic brain injury death rate, and found that “[alcohol] didn’t turn out to be as protective as the presence of the marijuana”.
More Evidence for Utility of Cannabinoid-Based Medicines
While the results of this study do not definitively prove that the use of cannabis (at levels resulting in physiologically detectable levels of THC) will help to prevent death in the case of a traumatic brain injury, they do lend to a growing body of evidence thatendogenous cannabinoids (i.e. those occurring naturally in our bodies, such as 2-AG) and exogenous cannabinoids (e.g. those found in the cannabis plant, or synthetic forms) may prevent or halt brain injury, even in infants.
 For instance, a 2013 study published in Neuropharmacology found that when administered to piglets who had sustained hypoxic-ischemic brain injury (i.e. caused by low oxygen), CBD (cannabidiol), one of the most frequently occurring compounds in cannabis, “exerts robust neuroprotective effects… modulating excitotoxicity, oxidative stress and inflammation.”
For instance, a 2013 study published in Neuropharmacology found that when administered to piglets who had sustained hypoxic-ischemic brain injury (i.e. caused by low oxygen), CBD (cannabidiol), one of the most frequently occurring compounds in cannabis, “exerts robust neuroprotective effects… modulating excitotoxicity, oxidative stress and inflammation.”A 2001 study published in Nature found that administration of 2-AG to mice that had sustained closed head injury prevented “secondary injury” that follows the primary closed head injury (e.g. it reduced the occurrence of brain edema, decreased size of the area of damage and death of cells in the hippocampus [an area of the brain involved in memory]) and improved recovery. According to an abcNEWS article on the study, “The cannabinoid, 2-AG, is believed to work in three ways. First, it reduces the levels of glutamate, a toxic molecule, released after injury. Second, it decreases the amount of free radicals and TNF (a chemical that induces inflammation) after injury. Third, it increases the blood supply to the brain. All three mechanisms are essential for limiting the damage done after the primary injury.”
In a 2006 study published in found that dexanabinol, a synthetic cannabinoid derivative, while found to be safe, was not effective in treating TBI (dexanabinol does not produce the intoxication caused by cannabis strains with psychoactive levels of THC because instead of binding to CB1 and CB2 receptors, it functions by blocking NMDA/glutamate receptors and neutralizing free radicals which can damage the body).
All of these findings signify a need for increased research into the effects of THC and other naturally occurring and synthetic cannabinoids on brain injury and as general neuroprotectiveagents, which may have roles in treatment of neurodegenerative diseases like ALS, Alzheimer’s, Parkinson’s, Huntington’s, and others.
For information on reasonable expectations and safety in considering whole-plant medical cannabis use, as well as how you can advocate to move cannabis out of the Schedule I controlled substance classification in order to increase research on phytocannabinoids in the United States, click here.
READ THE FULL ARTICLE HERE: http://www.medicaljane.com/2014/10/18/link-discovered-between-thc-and-decreased-traumatic-brain-injury-deaths/
Treating Cerebral Palsy Symptoms With Medical Marijuana

 Arielle GerardJuly 07, 2014
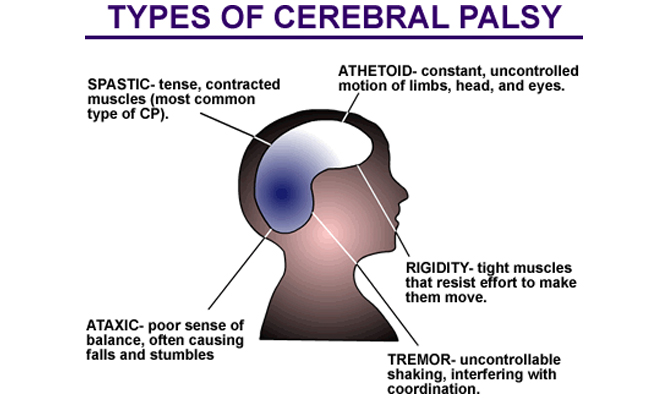
Arielle GerardJuly 07, 2014What Is Cerebral Palsy (CP)?
Patients with cerebral palsy may experience pain (often as a result of stiff muscles), incontinence, sleep disturbance, developmental, hearing, speech and vision impairments, andother signs and symptoms. 35%-50% of children with cerebral palsy develop seizure disorders. While the damage to the brain which causes cerebral palsy does not generally worsen or improve over time, signs and symptoms may change.
The exact cause of cerebral palsy in each individual case is somewhat unknown, although there are strong probable causes such as bleeding in the brain, lack of oxygen delivery to the brain, damage as a result of trauma, and infections.
Medical Marijuana & Cerebral Palsy
To date, no high-quality evidence (e.g. results from studies using double-blinding, a placebo control, and/or randomization) has been gathered assessing the effects of medical cannabis on patients with cerebral palsy. However, the potential for cannabis as medicine for patients with cerebral palsy has been explored in some measure in the medical community with promising results.
“Data has been gathered evidencing the efficacy of strains of cannabis with varying cannabinoid ratios in controlling symptoms of cerebral palsy.”
In a survey study on pain treatments used by patients with cerebral calsy, the researchers found, “The treatment that was rated as providing the most relief was marijuana; however, less than 5% of the sample reported ever using this drug for pain.”
One case study published in the Reviews in Neurological Diseases found that a 45-year old man with cerebral palsy and epilepsy showed “marked improvement with the use of marijuana”.
Additionally and importantly, data has been gathered on other conditions (such as multiple sclerosis), evidencing the potential efficacy of cannabis in controlling symptoms often experienced by patients with cerebral palsy, including spasticity, neuropathic pain,chronic pain, sleep disturbance, and seizures.
While definitive cause-effect relationships cannot be evaluated by case studies, and self-reported improvements can potentially be caused by the “placebo effect”, anecdotal evidence gathered from patients struggling with cerebral palsy should be strongly considered. Although anecdotal evidence and self-reports cannot be used as factual evidence, due to the real-world significance of patient evaluation in assessing and determining clinical improvements in symptoms such as spasticity and pain, patients’ self-reports should not be discounted by medical professionals.
In most cases and under medical supervision, the safety profile of whole-plant cannabis allows for safe experimentation by adult patients seeking relief that may be provided by cannabis use. The following videos detail the personal stories of individuals with cerebral palsy who have found benefit from medical cannabis use.
 Medical Marijuana May Help Manage Symptoms Of Cerebral Palsy
Medical Marijuana May Help Manage Symptoms Of Cerebral Palsy“Medical cannabis may be a potential add-on treatment option for the control of symptoms for patients with intractable symptoms which result from cerebral palsy.”
Cannabis has shown medical efficacy for symptoms such as spasticity, pain, and sleep disturbance in other conditions, and anecdotal evidence provides additional support for its use as a treatment option for cerebral palsy symptoms.
Given that cerebral palsy patients with intractable symptoms often need to explore other options when standard therapies fail, and that cannabis has a relatively low side-effect profile which allows for low-risk experimentation in most cases (under medical guidance), medical cannabis may be a potential add-on treatment option. More high-quality research needs to be conducted in order to assess whether or not cannabis is an effective treatment option for patients with cerebral palsy.
For information on reasonable expectations and safety in considering whole-plant medical cannabis use, as well as how you can advocate to move cannabis out of the Schedule I controlled substance classification in order to increase research on phytocannabinoids in the United States, click here.
A Look Into Mental Health and Medical Marijuana

 Arielle Gerard July 18, 2014
Arielle Gerard July 18, 2014One of the common questions relevant to the debate on medical marijuana use and legalization is, “How does cannabis affect mental illness?” To understand this question fully, it is necessary to understand some basics about the field of research, to assess the available evidence surrounding this question, and to consider the possible application of marijuana in treating symptoms of mental health conditions.
Why Do People Think Cannabis Causes Mental Illness?
Many studies have found that people who consume cannabis tend to be more likely to have various types of mental health issues, such as depression, anxiety, and psychotic disorders. As a result of these studies, people have incorrectly inferred that marijuana use causes mental illness.
However, this assumption stems from a basic misunderstanding of research results; namely, the fact that correlation does not imply causation. You may have heard this before. So what does it mean, and why does it matter?
Correlational vs. Cause-Effect Relationships
Correlation is a link or association that is found between two variables. There can be a negative correlation between variables, meaning that when one variable increases in magnitude/frequency, the other decreases in magnitude/frequency. For example, the more you exercise, the less likely you are to gain weight.
You can also have a positive correlation between variables, meaning that when one variable increases in magnitude/frequency, the other does so as well. For example, the more often you eat high-salt foods, the more likely you are to develop certain health problems such as high blood pressure.
However, a correlational relationship is not equivalent to a cause-effect relationship. That is to say, just because there is a correlation between two variables, it does not mean that one caused the other. For instance, one of the most frequently cited examples of when correlation does not imply causation goes as follows: In the summertime, ice cream sales increase, and murders also increase. So that means that when people buy more ice cream, this causes people to have an increased desire to go out and kill people, right? Wrong!
There could be a third, unseen factor causing both an increase in ice cream sales and murders— heat! As the heat rises, people like to eat cold foods/desserts (e.g. ice cream). Heat may also cause people to become more agitated, angry, and frustrated, and they are more frequently outdoors in close proximity with other individuals. All of this together can unfortunately result in an increased murder rate.
“This misunderstanding of correlational relationships is also partially responsible for the widely-held belief in the ‘gateway theory.'”
Correlational relationships can be helpful in assessing, understanding data, and can help develop research that will assess the possibility of a cause-effect relationship between variables. But a causative link between two variables cannot be drawn from the mere existence of a correlation between them.
 This misunderstanding of correlational relationships is also partially responsible for the widely-held belief in the “gateway theory”, which incorrectly asserts that cannabis use leads to a desire for more dangerous drugs, such as heroin or cocaine.
This misunderstanding of correlational relationships is also partially responsible for the widely-held belief in the “gateway theory”, which incorrectly asserts that cannabis use leads to a desire for more dangerous drugs, such as heroin or cocaine.
The Importance Of Understanding Selection Bias
The frequent conclusion that cannabis causes mental disorders, drawn from studies showing a link between marijuana use and mental illness, may be a directional misinterpretation. That is, it is very possible that users are more likely to utilize medical marijuana because they have a mental health disorder, and not that it actually leads to the development of mental health disorders. This can lead to a “selection bias” in studies.
According to one source, selection bias is defined by “systematic differences between comparison groups in prognosis or responsiveness to treatment”. Most studies conducted evaluating the impact of marijuana on mental illness have used recreational consumers as participants, and therefore begin the study with inherent selection bias.
Some people with mental disorders such as depression, anxiety, or psychotic mental disorders may choose to self-medicate with marijuana, individuals with schizophrenia may be more likely to use marijuana possibly due to their genetic makeup, and certain psychotic illnesses which already exist may be exacerbated by marijuana use. Therefore, the results of many studies which find links between marijuana use and mental health disorders do not provide sufficient evidence that marijuana causes mental illness; the group that consumes cannabis is likely inherently different than their counterparts from the outset of the study.
If there are differences between the two groups before the study has even begun, it is impossible to assess whether differing results for the two groups (i.e. mental illness or no mental illness) is due to cannabis use or due to some other factor that made the two groups different in the first place. Therefore, these studies using self-selected recreational consumers as participants do not provide valid evidence that cannabis causes mental illness.
Additionally, a recent retrospective study conducted at Harvard shows that marijuana use does not cause schizophrenia specifically.
So how can we definitively answer the question of whether or not marijuana causes mental illness? One of the highest quality study designs available to assess this question would employ a longitudinal design (i.e. the participants’ progress would be assessed over time, preferably for several years).
The researchers would randomly select individuals from a certain pool, thereby creating a group that is representative of the entire population. The representative sample would then be randomly divided into a “consumption” group or a control group that does not consume cannabis.
The consumption group would be assigned to use a certain amount of cannabis over time, whereas the control group would use none. After several years, the researchers would assess whether or not mental health issue incidence was different between the two groups.
There are few issues with conducting this type of study. For instance, these studies are of long duration, and therefore participant dropout rates may be high. Also, the legal status of marijuana as a Schedule I controlled substance and ethical considerations may limit the ability for researchers to undertake such a study.
Cannabis with an approximated THC content of at least 2% often produces psychoactive effects when inhaled or ingested. Examples of these potential effects include euphoria, paranoia, anxiety, depression, a distorted sense of time, magical thinking.
While there is a low risk of dependence with marijuana use, tolerance and withdrawal symptoms do exist. Their effects are generally mild, but this suggests that there is potential for both a psychological and physiological dependence in some users. When necessary to decrease dosage and frequency of medical marijuana, tapering is suggested and may minimize the experience of withdrawal. Symptoms of cannabis withdrawal include irritability, anxiety, and sleep disturbance.
“Ideally, medical marijuana should be used under the supervision of a medical professional so that any progress and potentially harmful side effects can be continually monitored and addressed.”
The experiences of an altered mental state, potentially caused by intoxication and withdrawal, are short in duration and there is no evidence to suggest that they are the result of an underlying mental illness caused by cannabis consumption.
However, there is some evidence to suggest that cannabis use may exacerbate certain underlying mental health conditions in both adults and adolescents. In the review “Medical Marijuana: Clearing Away the Smoke”, Grant et al. state the following: “Although unlikely to be a factor in the application of cannabinoids for pain, there is concern that early adolescent use of cannabis may heighten later risk of psychosis, and evidence that genetic variation (single nucleotide polymorphisms) heightens vulnerability.”
Additionally, it has been suggested, though not proven, that cannabis may interrupt proper brain development if use begins early in life. For this reason, medical marijuana should primarily be used by adolescent patients only when their condition is severely debilitating and other treatments are ineffective, or have a highly unfavorable side-effect profile. Ideally, medical marijuana should be used under the supervision of a medical professional so that progress and potentially harmful side effects can be continually monitored and addressed.
Not only is there a lack of valid and reliable evidence in support of the statement that marijuana causes mental illness, but cannabinoids and whole-plant marijuana actually may be useful as a treatment option for certain mental health issues. These include anxiety, general psychosis, schizophrenia (1, 2), depression, social anxiety disorder (SAD), obsessive compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and alcoholism and addiction.
“There is ample existing scientific and anecdotal evidence suggesting that marijuana can help reduce PTSD symptoms. However, the clinical research hasn’t been allowed to happen yet.” – Rick Doblin
According to MAPS founder and executive director Rick Doblin, PhD, “There is ample existing scientific and anecdotal evidence suggesting that marijuana can help reduce PTSD symptoms. However, the clinical research hasn’t been allowed to happen yet. For example, pure THC has been shown to reduce PTSD-like behavior in animals, and survey research clearly shows that thousands of people with PTSD use marijuana to cope with PTSD symptoms. In order to discover the real safety and therapeutic effectiveness of marijuana in humans with PTSD, we need clinical trials comparing subjects using marijuana to those using no marijuana, and to those using different strains with various combinations of THC and CBD, which has anti-anxiety properties.”
While relatively rare, some individuals who develop a problematic dependence on marijuana may need counseling in order to help them find alternative coping methods. However, due to the debilitation associated with these disorders, difficulties in treatment, and the safety profile of cannabis use, investigation into its relevance as a potential treatment option for mental health issues is needed.
Much more research needs to be conducted in this area before it can be stated that medical marijuana is a useful treatment for mental health conditions or their symptoms. However, the preliminary data does provide additional evidence to justify a strong challenging of the blanket statement that “marijuana causes mental illness”.
Conclusion
Despite the need for more research, the data gathered thus far does not provide sufficient evidence to suggest that cannabis causes mental illness. In fact, it may even be useful as an adjunct therapy for the treatment of certain mental health disorders or their symptoms.
However, due to the possible exacerbation of psychotic mental illness that medical marijuana has the potential to cause, it should be used under the supervision of a physician who is aware of the patient’s current physical status and full medical (including mental health, family, and social) history.
If medical marijuana patients begin to notice any unusual changes in mood, behavior, thinking, speech, memory, or any other unusual symptoms, they are encouraged to speak with their healthcare provider immediately.
Main Reference: “Understanding Marijuana” by Dr. Mitch Earleywine
There could be a third, unseen factor causing both an increase in ice cream sales and murders— heat! As the heat rises, people like to eat cold foods/desserts (e.g. ice cream). Heat may also cause people to become more agitated, angry, and frustrated, and they are more frequently outdoors in close proximity with other individuals. All of this together can unfortunately result in an increased murder rate.
“This misunderstanding of correlational relationships is also partially responsible for the widely-held belief in the ‘gateway theory.'”
Correlational relationships can be helpful in assessing, understanding data, and can help develop research that will assess the possibility of a cause-effect relationship between variables. But a causative link between two variables cannot be drawn from the mere existence of a correlation between them.
 This misunderstanding of correlational relationships is also partially responsible for the widely-held belief in the “gateway theory”, which incorrectly asserts that cannabis use leads to a desire for more dangerous drugs, such as heroin or cocaine.
This misunderstanding of correlational relationships is also partially responsible for the widely-held belief in the “gateway theory”, which incorrectly asserts that cannabis use leads to a desire for more dangerous drugs, such as heroin or cocaine.The Importance Of Understanding Selection Bias
The frequent conclusion that cannabis causes mental disorders, drawn from studies showing a link between marijuana use and mental illness, may be a directional misinterpretation. That is, it is very possible that users are more likely to utilize medical marijuana because they have a mental health disorder, and not that it actually leads to the development of mental health disorders. This can lead to a “selection bias” in studies.
According to one source, selection bias is defined by “systematic differences between comparison groups in prognosis or responsiveness to treatment”. Most studies conducted evaluating the impact of marijuana on mental illness have used recreational consumers as participants, and therefore begin the study with inherent selection bias.
Some people with mental disorders such as depression, anxiety, or psychotic mental disorders may choose to self-medicate with marijuana, individuals with schizophrenia may be more likely to use marijuana possibly due to their genetic makeup, and certain psychotic illnesses which already exist may be exacerbated by marijuana use. Therefore, the results of many studies which find links between marijuana use and mental health disorders do not provide sufficient evidence that marijuana causes mental illness; the group that consumes cannabis is likely inherently different than their counterparts from the outset of the study.
If there are differences between the two groups before the study has even begun, it is impossible to assess whether differing results for the two groups (i.e. mental illness or no mental illness) is due to cannabis use or due to some other factor that made the two groups different in the first place. Therefore, these studies using self-selected recreational consumers as participants do not provide valid evidence that cannabis causes mental illness.
Additionally, a recent retrospective study conducted at Harvard shows that marijuana use does not cause schizophrenia specifically.
How To Measure The Connection Between Cannabis, Mental Illness
So how can we definitively answer the question of whether or not marijuana causes mental illness? One of the highest quality study designs available to assess this question would employ a longitudinal design (i.e. the participants’ progress would be assessed over time, preferably for several years).
The researchers would randomly select individuals from a certain pool, thereby creating a group that is representative of the entire population. The representative sample would then be randomly divided into a “consumption” group or a control group that does not consume cannabis.
The consumption group would be assigned to use a certain amount of cannabis over time, whereas the control group would use none. After several years, the researchers would assess whether or not mental health issue incidence was different between the two groups.
There are few issues with conducting this type of study. For instance, these studies are of long duration, and therefore participant dropout rates may be high. Also, the legal status of marijuana as a Schedule I controlled substance and ethical considerations may limit the ability for researchers to undertake such a study.
Intoxication, Withdrawal, And Exacerbation
Cannabis with an approximated THC content of at least 2% often produces psychoactive effects when inhaled or ingested. Examples of these potential effects include euphoria, paranoia, anxiety, depression, a distorted sense of time, magical thinking.
While there is a low risk of dependence with marijuana use, tolerance and withdrawal symptoms do exist. Their effects are generally mild, but this suggests that there is potential for both a psychological and physiological dependence in some users. When necessary to decrease dosage and frequency of medical marijuana, tapering is suggested and may minimize the experience of withdrawal. Symptoms of cannabis withdrawal include irritability, anxiety, and sleep disturbance.
“Ideally, medical marijuana should be used under the supervision of a medical professional so that any progress and potentially harmful side effects can be continually monitored and addressed.”
The experiences of an altered mental state, potentially caused by intoxication and withdrawal, are short in duration and there is no evidence to suggest that they are the result of an underlying mental illness caused by cannabis consumption.
However, there is some evidence to suggest that cannabis use may exacerbate certain underlying mental health conditions in both adults and adolescents. In the review “Medical Marijuana: Clearing Away the Smoke”, Grant et al. state the following: “Although unlikely to be a factor in the application of cannabinoids for pain, there is concern that early adolescent use of cannabis may heighten later risk of psychosis, and evidence that genetic variation (single nucleotide polymorphisms) heightens vulnerability.”
Additionally, it has been suggested, though not proven, that cannabis may interrupt proper brain development if use begins early in life. For this reason, medical marijuana should primarily be used by adolescent patients only when their condition is severely debilitating and other treatments are ineffective, or have a highly unfavorable side-effect profile. Ideally, medical marijuana should be used under the supervision of a medical professional so that progress and potentially harmful side effects can be continually monitored and addressed.
Cannabis As A Potential Treatment For Certain Mental Illnesses
Not only is there a lack of valid and reliable evidence in support of the statement that marijuana causes mental illness, but cannabinoids and whole-plant marijuana actually may be useful as a treatment option for certain mental health issues. These include anxiety, general psychosis, schizophrenia (1, 2), depression, social anxiety disorder (SAD), obsessive compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and alcoholism and addiction.
“There is ample existing scientific and anecdotal evidence suggesting that marijuana can help reduce PTSD symptoms. However, the clinical research hasn’t been allowed to happen yet.” – Rick Doblin
According to MAPS founder and executive director Rick Doblin, PhD, “There is ample existing scientific and anecdotal evidence suggesting that marijuana can help reduce PTSD symptoms. However, the clinical research hasn’t been allowed to happen yet. For example, pure THC has been shown to reduce PTSD-like behavior in animals, and survey research clearly shows that thousands of people with PTSD use marijuana to cope with PTSD symptoms. In order to discover the real safety and therapeutic effectiveness of marijuana in humans with PTSD, we need clinical trials comparing subjects using marijuana to those using no marijuana, and to those using different strains with various combinations of THC and CBD, which has anti-anxiety properties.”
While relatively rare, some individuals who develop a problematic dependence on marijuana may need counseling in order to help them find alternative coping methods. However, due to the debilitation associated with these disorders, difficulties in treatment, and the safety profile of cannabis use, investigation into its relevance as a potential treatment option for mental health issues is needed.
Much more research needs to be conducted in this area before it can be stated that medical marijuana is a useful treatment for mental health conditions or their symptoms. However, the preliminary data does provide additional evidence to justify a strong challenging of the blanket statement that “marijuana causes mental illness”.
Conclusion
Despite the need for more research, the data gathered thus far does not provide sufficient evidence to suggest that cannabis causes mental illness. In fact, it may even be useful as an adjunct therapy for the treatment of certain mental health disorders or their symptoms.
However, due to the possible exacerbation of psychotic mental illness that medical marijuana has the potential to cause, it should be used under the supervision of a physician who is aware of the patient’s current physical status and full medical (including mental health, family, and social) history.
If medical marijuana patients begin to notice any unusual changes in mood, behavior, thinking, speech, memory, or any other unusual symptoms, they are encouraged to speak with their healthcare provider immediately.
Main Reference: “Understanding Marijuana” by Dr. Mitch Earleywine
Subscribe to:
Comments (Atom)


